What's the Vaginal Microbiome Got To Do With It?
- Alexandra O'Connor
- Oct 5, 2021
- 7 min read
Updated: Feb 4, 2022
WHAT HAS THE VAGINAL MICROBIOME GOT TO DO WITH IT?
A LOT!!
In my experience the health of the vaginal microbiome is rarely investigated by GPs and IVF clinics, even when there are clear signs and symptoms that things may not all be as healthy as they could be down there.
In my clinic, these are some of the things that would make me think that we need to dig a little bit deeper in this area:
a history of recurrent 'thrush like symptoms' (even if it was years ago and hasn't been an issue recently)
intermittent or regular vaginal discharge - either at certain times of the cycle, or after antibiotics etc
intermittent or regular soreness or itching of the vulva or vagina
if someone mentions that they notice their knickers 'bleaching' from contact with a vaginal discharge
a history of cystitis or urinary tract infections (UTIs)
recurrent implantation failure
long term unexplained infertility
a history of frequent or strong antibiotic use
WHAT IS THE VAGINAL MICROBIOME
The vaginal microbiome is a dynamic micro-ecosystem that exists within the vagina. This ecosystem fluctuates and flexes through the different phases of the menstrual cycle and plays a vital role in maintaining a healthy, sperm-friendly, infection resisting environment that will support fertility.
Under normal circumstances around of the microbes in the vaginal microbiome are different strains of protective lactobacillus 95%, the remainder of the space contains yeasts, fungi and other commensal bacteria. Commensal bacteria can be tolerated and can be beneficial in low numbers, but if their population explodes they become pathological - they can cause inflammation, change the pH of the vagina which can cause tissue damage and can change the way some of the cells lining the vagina behave. It is thought that they can also infect sperm, and it is possible for these bacteria to move on upwards through the cervix into the uterus and beyond.
VAGINAL MICROBIOME ISSUES CAN IMPACT FERTILITY
A healthy vaginal microbiome creates an environment that is sperm friendly. It also acts as a buffer between the outside world and the uterine environment, ensuring that no pathological microbes make their way up towards the uterus and ovaries.
If the vaginal microbiome is out of balance, it can impact so many aspects of fertility:
It can impact sperm survival
it can change the behaviour of some cells to have an impact on our ability to create sperm-supportive cervical mucus
it can alter the pH of the vaginal cavity which can make the environment more attractive to pathogenic microbes
it can cause the vagina to become a reservoir of inflammation and pathogenic bacteria which can have a negative impact on the health of the uterine environment and even the ovarian environment
it raises the risk of developing pelvic inflammatory disease
THE VAGINAL MICROBIOME IMPACTS PREGNANCY TOO
The vaginal microbiome is not only important for fertility, but it also plays a surprisingly important role in pregnancy. A disrupted vaginal microbiome has been found to be associated with issues such as shortening cervix during pregnancy and preterm birth. The best time to prepare the vaginal microbiome for pregnancy is BEFORE pregnancy.
WHAT ARE THE MOST COMMON VAGINAL MICROBIOME ISSUES
When it comes to the vaginal microbiome, the main concerns are thrush (candida) or BV (bacterial vaginosis). It isn't always easy to tell which is which based on symptoms, and both should be treated differently.
The main different types of vaginal discharge are as follows:
BACTERIAL VAGINOSIS (BV)
This typically presents as a thin mucus discharge, white, grey or greenish with a fishy odour.
This discharge is usually, but not always accompanied by burning, itching, pain and swelling of the vagina.
Bacterial vaginosis will usually raise the pH of the vagina, making it more susceptible to further infection, bacterial overgrowth and STIs.
The vagina is a natural home to a wide range of other microbes, but these are normally held at bay by the protective lactobacillus bacteria. If there is a drop in lactobacillus, or if the lactobacillus becomes overwhelmed by an external pathogen then a state of bacterial vaginosis will occur.
Around 50% of women with bacterial vaginosis will have no obvious symptoms.
Bacterial vaginosis often requires treatment with antibiotics followed by a supportive regime to restore a healthy vaginal microbiome.
VULVOVAGINAL CANDIDIASIS (thrush)
This typically presents as a thick, lumpy white discharge - a bit like cottage cheese
There is often no particular odour though the discharge may smell a bit yeasty.
This is usually accompanied by burning or itching sensations, redness and an itchy rash on the vulva.
Vaginal Candidiasis is common around ovulation.
This is often treated with over the counter antifungal treatments. Invivo Healthcare have a good therapeutic for thrush, BioMe FemmeC.
It is important not to keep treating recurrent thrush without testing to see what you are treating - it is possible for similar symptoms to occur from Cytolytic Vaginosis (see below).
CYTOLITIC VAGINOSIS
This presents in a similar way to thrush with an intermittent white discharge and itching. Under normal circumstances Lactobacillus species of bacteria produce acid which is protective and supportive of a healthy vaginal microbiome, but if someone has had repeated treatment for thrush-like symptoms it is possible for treatment to wipe out the natural opposition to lactobacillus, so there are not enough alkali producers to balance out the acid produced by the lactobacillus. This causes the pH to fall as the environment becomes more acidic than it should and this acidity can cause soreness, itching and burning pain after sex.
One of the giveaways for this infection is that it often appears to worsen in the days prior to the period starting (when there are even more lactobacillus than usual, producing more acid), and will be eased by onset of the period (which neutralises the acid).
Cytolytic vaginosis doesn't respond properly to thrush treatment - treatment may have a short-term benefit, but the infection will return soon after and the overall impact is actually to worsen the situation by decreasing the natural opposition to Lactobacillus.
This can often be improved by the use of a baking soda douche or bath which can help neutralise the acid and return the environment to state which will encourage better diversity of microbes.
If we are not sure of what we are dealing with, a vaginal microbiome test is a good place to start . . .
WHY A NORMAL VAGINAL CULTURE IS NOT PROOF THAT THERE THE VAGINAL ENVIRONMENT IS HEALTY
When a vaginal swab is sent for culture, the process involves taking a swab of the vagina, and sending this to a laboratory for testing. Any microbes found on the swab are grown in the laboratory so that the type and strain of microbe can be identified.
It is not unusual for someone with symptoms of a vaginal microbiome issue to be told by their GP that the culture was clear and that there is nothing to worry about. There are a few reasons why this can happen:
if the microbes on the swab don't survive the journey to the lab, they will not be alive to grow in the culture medium.
if the lab has been instructed to look for a restricted list of pathogens (such as chlamydia, gonorrhoea etc), then any other pathogen that grows is ignored (sometimes the report will have a comment on there about 'other unidentified growth seen'.
a vaginal culture does not usually report any information about the state of the good bacteria - it doesn't indicate if there are enough lactobacillus present or if there is a good range of different lactobacilli or is the environment being dominated by a single strain.
HOW DO I PREFER TO TEST THE VAGINAL MICROBIOME
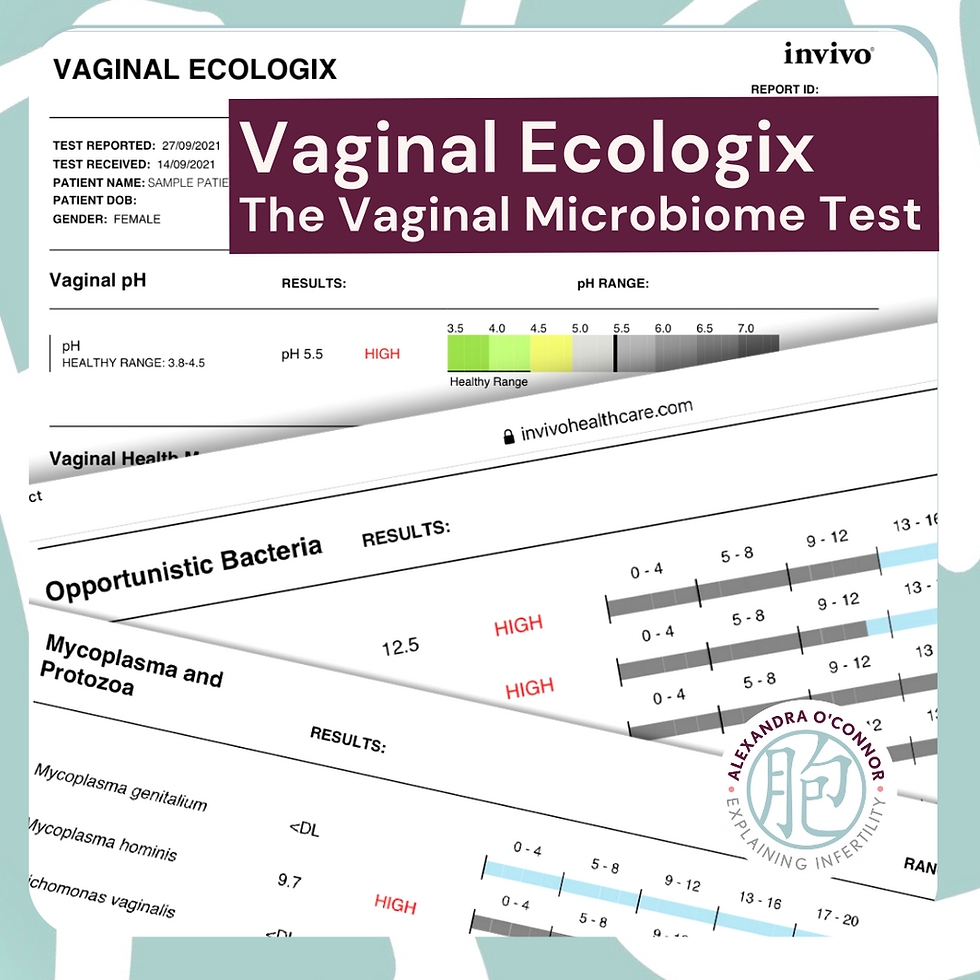
I work with the INVIVO VAGINAL MICROBIOME TEST, this is a PCR based test that provides a much fuller picture of the state of the vaginal microbiome. Using the results from this test get a much better indication of the state of the vaginal microbiome and enables us to target support for it, whether that is simply to improve the microbiome, or whether there are pathogens or commensal overgrowths that need to be treated.
The test looks at the microbiome in depth, looks at how the microbiome is balanced, whether all the key players are present or missing, look for pathological bacteria, yeasts and fungi, look at indicators of inflammation, infection etc.
While it is possible to opt to try to resolve a vaginal microbiome issue without testing, that is not such a good option. For example, if you were to diagnose BV when the issue is thrush, or thrush when the issue is cytolytic vaginosis, you might notice short term relief but would actually be worsening the situation.
Once we know what we are dealing with, the main vaginal therapeutic options are:
Invivo Healthcare BioMe FemmeV
This is the main option for bacterial vaginosis. It can be taken orally, but if a test result showed the lactobacillus populations were very low, I might advise the capsules are used vaginally for a week before using them orally.
Invivo Healthcare BioMe FemmeC
If thrush was more of an issue than BV, I would consider this option.
I may also recommend FemmeV in addition if the test results indicated it would help to build a healthier, more fertile vaginal microbiome.
Invivo Healthcare Biome FemmeUT
This is more appropriate if there is a history of recurrent urinary tract infections or an Ecoli overgrowth which is typically associated with recurrent UTIs.
To order the Vaginal Ecologix test or any of the Invivo therapeutics you will need to work with a doctor or practitioner registered with Invivo Healthcare (such as myself).
Research articles of interest
Characterizing the gut microbiota in females with infertility and preliminary results of a water soluble dietary fiber intervention studyShinnosuke Komiya, Yuji Naito, Hidetaka Okada, Yoshiyuki Matsuo, Kiichi Hirota, Tomohisa Takagi, Katsura Mizushima, Ryo Inoue, Aya Abe and Yoshiharu Morimoto
Potential Influence of the Microbiome on Infertility and Assisted Reproductive TechnologyIdo Sirota, Shvetha M. Zarek, and James H. Segars
The vaginal microbiome and preterm birthJennifer M. Fettweis, Myrna G. Serrano, Gregory A. Buck
Vaginal microbiome in early pregnancy and subsequent risk of spontaneous preterm birth: a case–control studyN Tabatabaei,AM Eren,LB Barreiro,V Yotova,A Dumaine,C Allard,WD Fraser
Persistent microbial dysbiosis in preterm premature rupture of membranes from onset until deliveryElizabeth A. Baldwin, Marina Walther-Antonio, Allison M. MacLean, Daryl M. Gohl, Kenneth B. Beckman, Jun Chen, Bryan White, Douglas J. Creedon, Nicholas Chia
Vaginal dysbiosis increases risk of preterm fetal membrane rupture, neonatal sepsis and is exacerbated by erythromycinRichard G. Brown, Julian R. Marchesi, Yun S. Lee, Ann Smith, Benjamin Lehne, Lindsay M. Kindinger, Vasso Terzidou, Elaine Holmes, Jeremy K. Nicholson, Phillip R. Bennett & David A. MacIntyre
The interaction between vaginal microbiota, cervical length, and vaginal progesterone treatment for preterm birth riskLindsay M. Kindinger, Phillip R. Bennett, Yun S Lee, Julian R. Marchesi, Ann Smith, Stefano Cacciatore, Elaine Holmes, Jeremy K. Nicholson, T. G. Teoh & David A. MacIntyre
Relationship between vitamin D status and the vaginal microbiome during pregnancyKimberly K. Jefferson, Hardik I. Parikh, Erin M. Garcia, David J. Edwards, Myrna G. Serrano, Martin Hewison, Judith R. Shary, Anna M. Powell, Bruce W. Hollis, Jennifer M. Fettweis, Jerome F. Strauss III, Gregory A. Buck & Carol L. Wagner
Prospective observational study of vaginal microbiota pre- and post-rescue cervical cerclageRG Brown,D Chan,V Terzidou,YS Lee,A Smith,JR Marchesi,DA MacIntyre,PR Bennett

.png)

Comments